Transforming Emergency Department Experiences for Rural Hospitals
VCU Health Innovation Lab • 2024
Challenge
In rural hospital emergency departments, long wait times are common due to limited resources and high patient volumes. This often leads to frustration and dissatisfaction among patients, with many leaving without receiving care. Our goal was to transform the waiting experience to make patients feel more cared for and reduce their perception of the wait.
Our Goal
To redesign the waiting experience in the emergency department by improving communication and comfort, ultimately reducing patient frustration and enhancing satisfaction.
My Role
As the Health Innovation Lab’s Research Lead, I conducted field studies, empathy interviews, and journey mapping sessions to capture the needs of patients and staff. I also co-instructed a course, Designing the Future of Health, which empowered students to address these real-world challenges in rural health systems through systems thinking and design innovation.
Learn more about the VCU da Vinci Center for Innovation.
Defining the Problem
Rural emergency departments face significant challenges in patient satisfaction due to long and sometimes unpredictable wait times. While medical attention was prioritized based on urgency, from empathy interviews and observation, we learned that communication gaps left patients feeling neglected, adding to frustration and prompting some to leave prematurely.
Research Approach
Interviews
I wrote the discussion guides for my team and our students to interview healthcare providers, staff, and leadership who worked in or interfaced with the emergency departments. The goal of this was to understand what other factors might be contributing to patient wait times or poor patient experiences when visiting the ED.
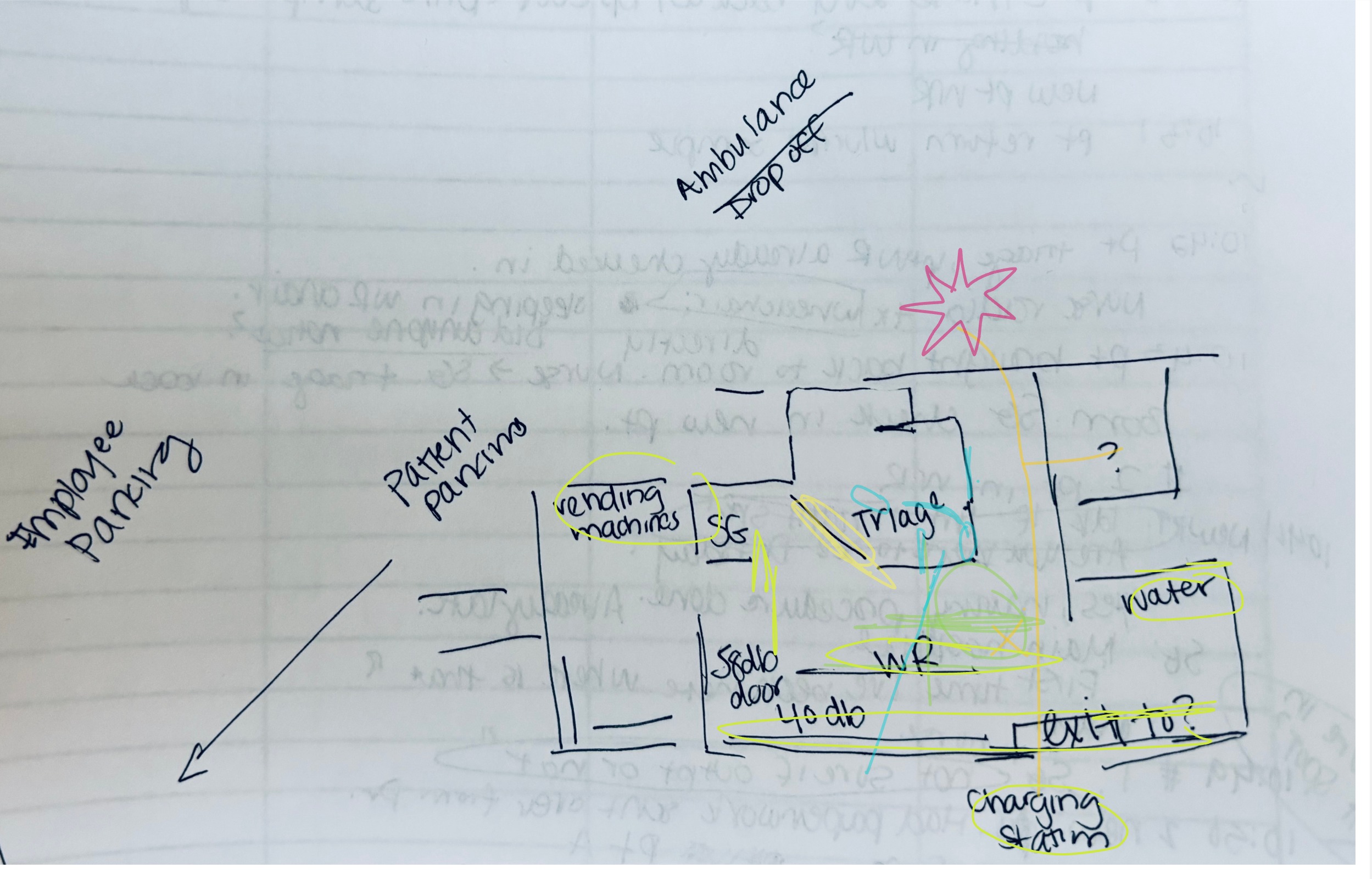
Observation
Through observation studies in the waiting rooms, we learned that patients often felt "forgotten" during their wait, with limited information about delays or expected treatment times. This lack of connection heightened stress and frustration.
Storyboarding
I drew storyboards based on the observation study experiences to highlight key opportunity areas. This allowed students to visualize potential scenarios for improving the patient experience in the ED waiting area, focusing on communication and comfort.
Journey Mapping
I mapped the patient journey from arrival to discharge, identifying moments where communication and comfort could be improved. The journey map highlighted critical touchpoints where brief interactions, like periodic check-ins from staff, could improve the perception of care and reduce anxiety. These insights provided a framework for targeted solutions to enhance patient comfort during their stay.
.jpg)
Core Question
How might we make patients feel even more cared for during their wait, and reduce the perception of wait time?
In the next phase, students brainstormed together with healthcare providers, staff, and leadership, encouraging a collaborative approach to generating potential solutions. Through ideation workshops we focused on brainstorming practical, low-cost interventions that address the systemic issues uncovered during the research phase. Ideas ranged from improving communication between staff and patients to developing new digital tools for tracking patient flow.

Kicking off our Innovation Kickoff, where students shared key insights and leverage points to help build a shared understanding of the problem space.
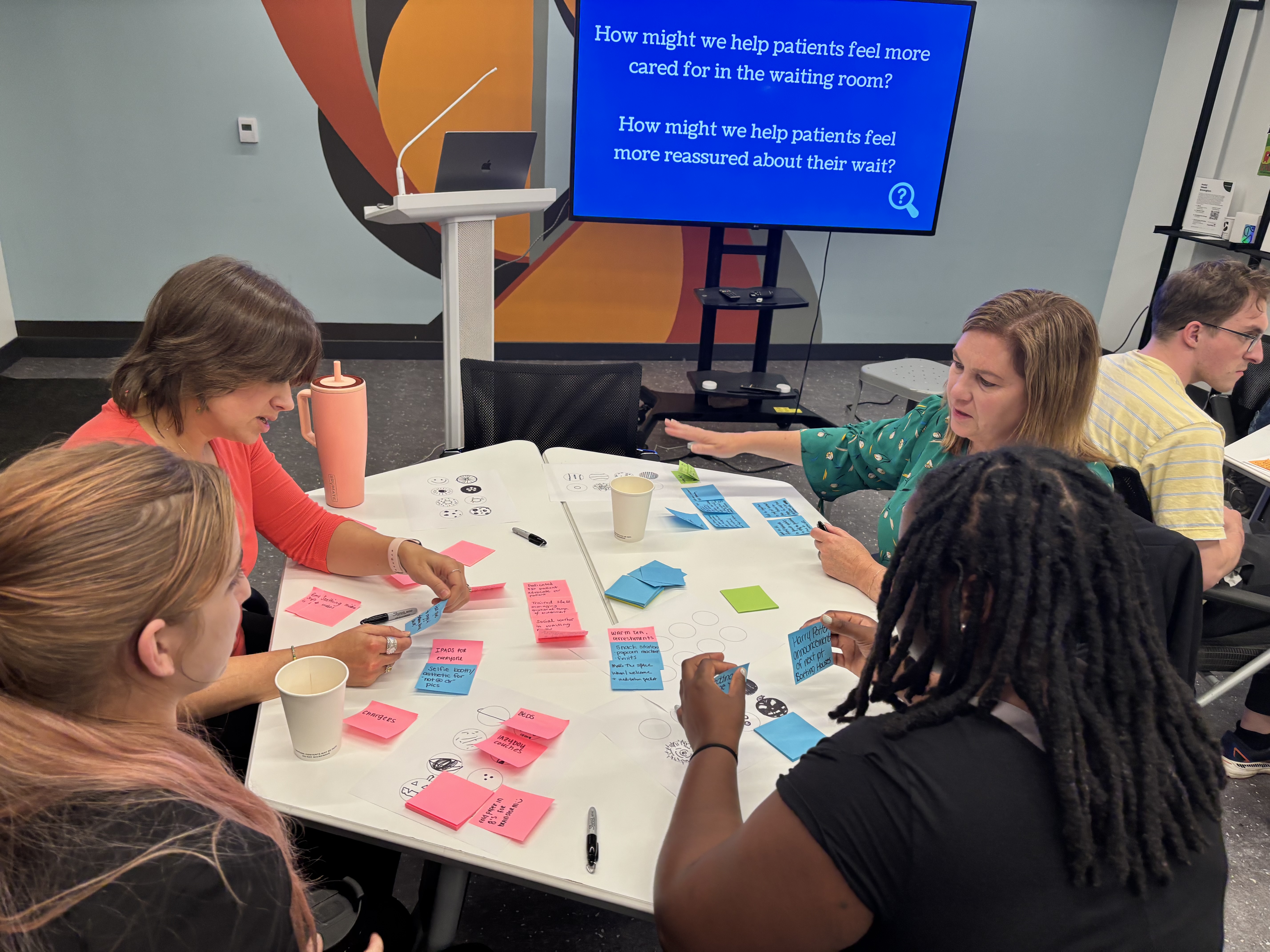
Students brainstormed alongside healthcare providers, staff, leadership, and community members to ensure many perspectives were included.
Prototyping and Iterative Testing
With ideas in hand, students develop prototypes that are tested and refined in collaboration with hospital staff. This hands-on process allows students to iterate based on feedback and real-world use. Solutions are designed to be implementable within the constraints of rural healthcare, ensuring that they are scalable and sustainable over time.
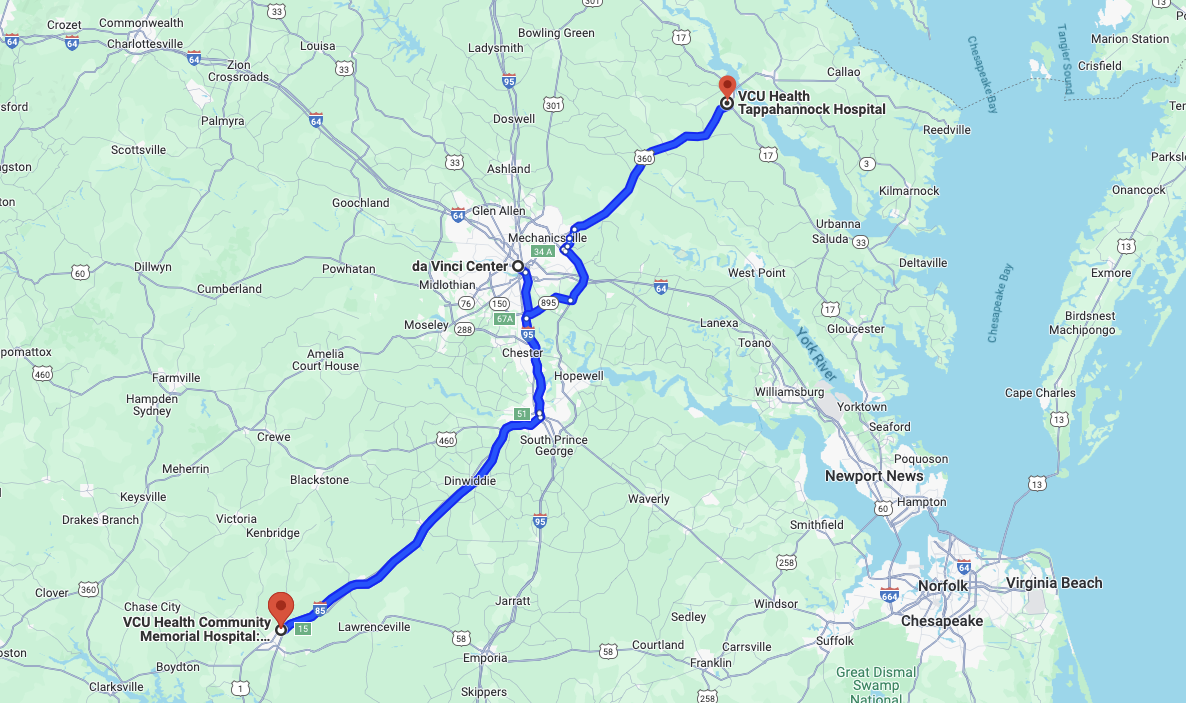
Insights are shared across both hospital sites, each of which has unique needs.

The VCU da Vinci Center Maker Space is a hub for hands-on innovation, offering students cutting-edge tools and resources to prototype, create, and bring ideas to life.
Reflection
This project highlighted the power of small, empathy-driven changes in healthcare design. By addressing patients' emotional needs and improving communication, we transformed the waiting experience, making patients feel valued and cared for even during long waits.
Key takeaways:
- Systems thinking. We utilized a systems thinking approach to gain a comprehensive understanding of the intricate challenges within our local health systems, enabling more effective and sustainable solutions.
- Student empowerment. Students took the lead on developing strategies to reducing the number of patients leaving without being seen in rural community hospital emergency departments, which made for powerful networking and career development opportunities.
- Health system collaboration. The partnership between students and rural healthcare providers fosters a culture of innovation in these hospitals, demonstrating that even small changes can have a big impact.