Emergency Department Challenge
Discovery research to identify opportunities to help patient get the treatment they need in rural emergency departments.
Reducing Patient Walk-Outs in Rural Emergency Departments
In rural hospital emergency departments, long wait times are a common challenge that lead to patient frustration, dissatisfaction, and, often, patients leaving without receiving care. This case study details a research initiative aimed at improving the waiting experience for patients, enhancing communication, and making care feel more accessible. Through field studies, empathy interviews, and journey mapping, we uncovered key pain points in the emergency department environment and identified creative strategies to transform these experiences. By focusing on systems thinking, collaboration, and low-cost interventions, this project resulted in measurable improvements in patient satisfaction, highlighting how simple yet effective changes can drive lasting impact in rural healthcare settings.
Client
VCU Health
Timeframe
Sep - Dec 2024
Role
Lead UX Researcher
Challenge
At two of VCU Health's rural community hospitals, long wait times in emergency departments led to increased patient frustration and a high rate of patients leaving without being seen. Hospital leadership was invested in sharing patient outcomes data and feedback through daily huddles but struggled to create lasting improvements in patient experience. My role was to lead the research efforts to uncover patient and staff pain points, analyze systemic inefficiencies, and design actionable solutions to improve communication and perceived wait times.
Introducing the SmartWait app: Connecting patients to emergency care when they need it most. This is a mid-fidelity prototype I designed in Figma based on an innovative student team's concept that enables patients to begin their care journey before physically arriving at the emergency department. I've enhanced the design with a new feature that connects patients directly to a dedicated care advocate who can provide real-time information about wait times, facility directions, and set clear expectations for their visit.
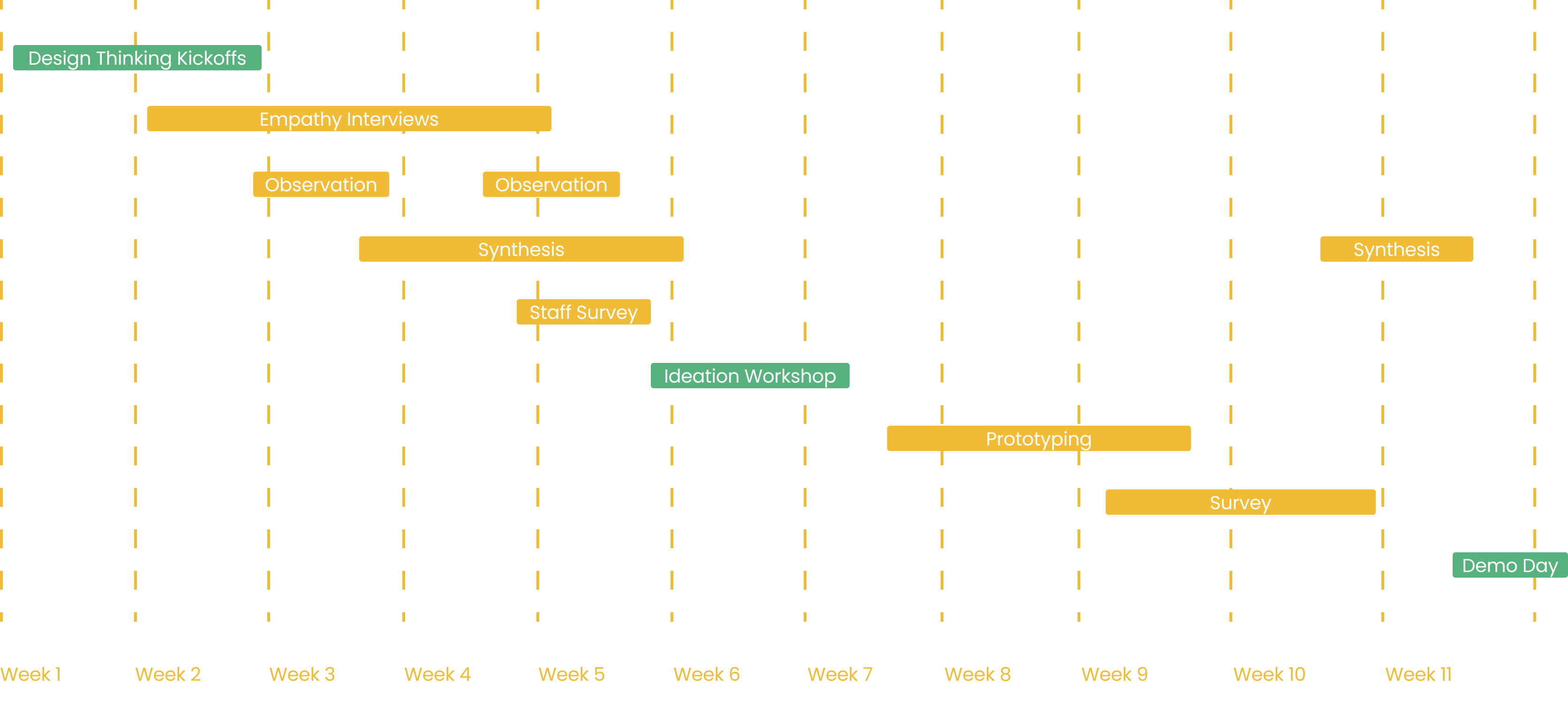
The Research Process
To build a deep understanding of patient and staff experiences, I led a comprehensive mixed-methods research study, incorporating:
- Field observations. Conducted in-person observations in emergency department waiting rooms, analyzing staff-patient interactions, environmental stressors, and bottlenecks in the care process.
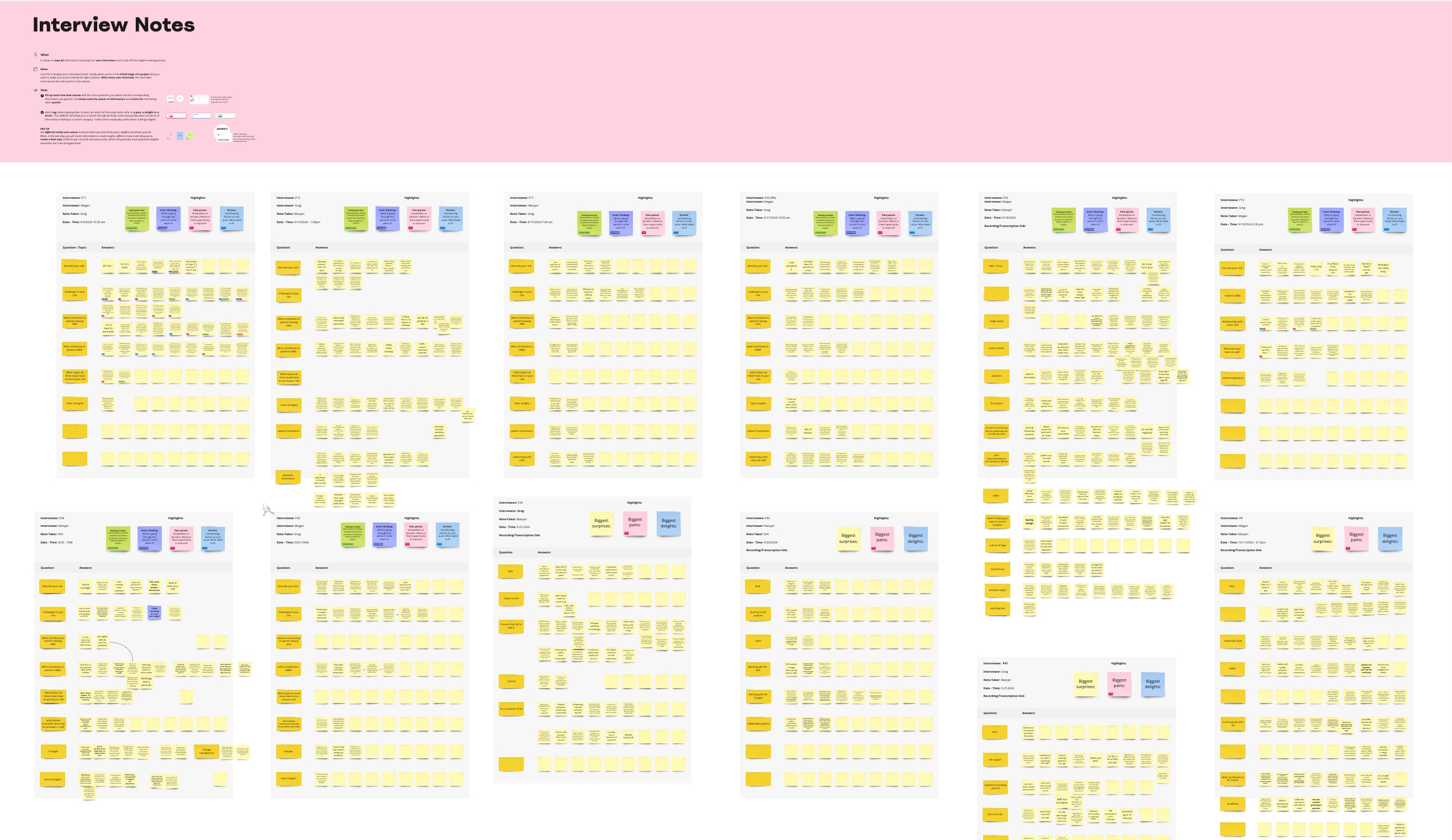
- Semi-structured interviews. Designed, helped facilitate, and analyzed, 18 interviews with a diverse set of stakeholders—including emergency techs, nurses, physicians, and hospital presidents—to understand their perspectives on operational challenges and communication breakdowns. Crafting interview guides for this broad range of roles was particularly challenging, requiring careful adaptation of questions to uncover relevant insights across all levels of hospital leadership.
- Survey design & analysis. Developed and administered surveys for staff and providers to assess perceptions of design challenges and prototype concepts.
- Collaborative synthesis & insight generation. Led co-synthesis sessions using affinity mapping and journey mapping techniques to distill research findings into key themes that informed solution development.
.jpg)
Key Observation Insights
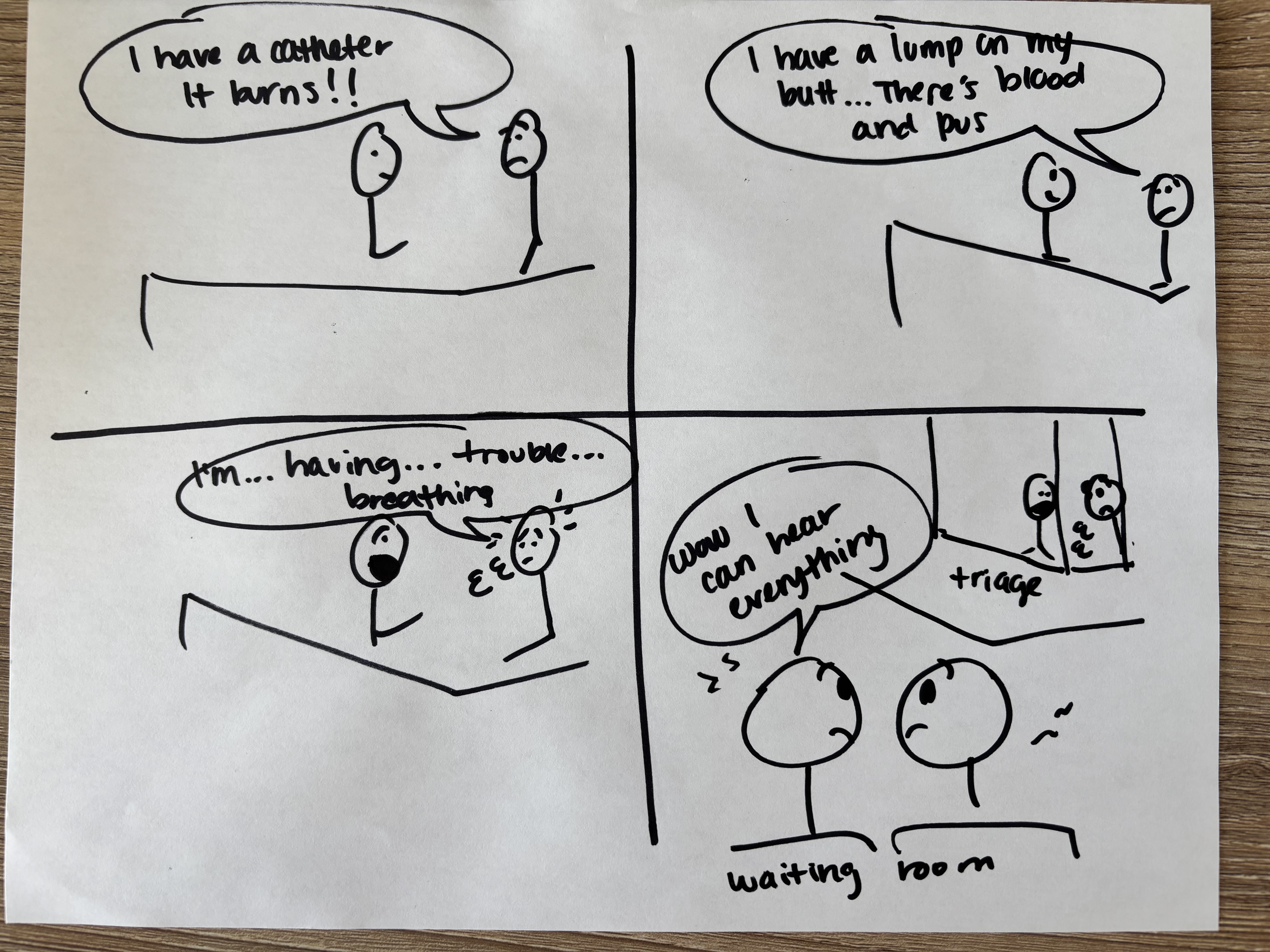
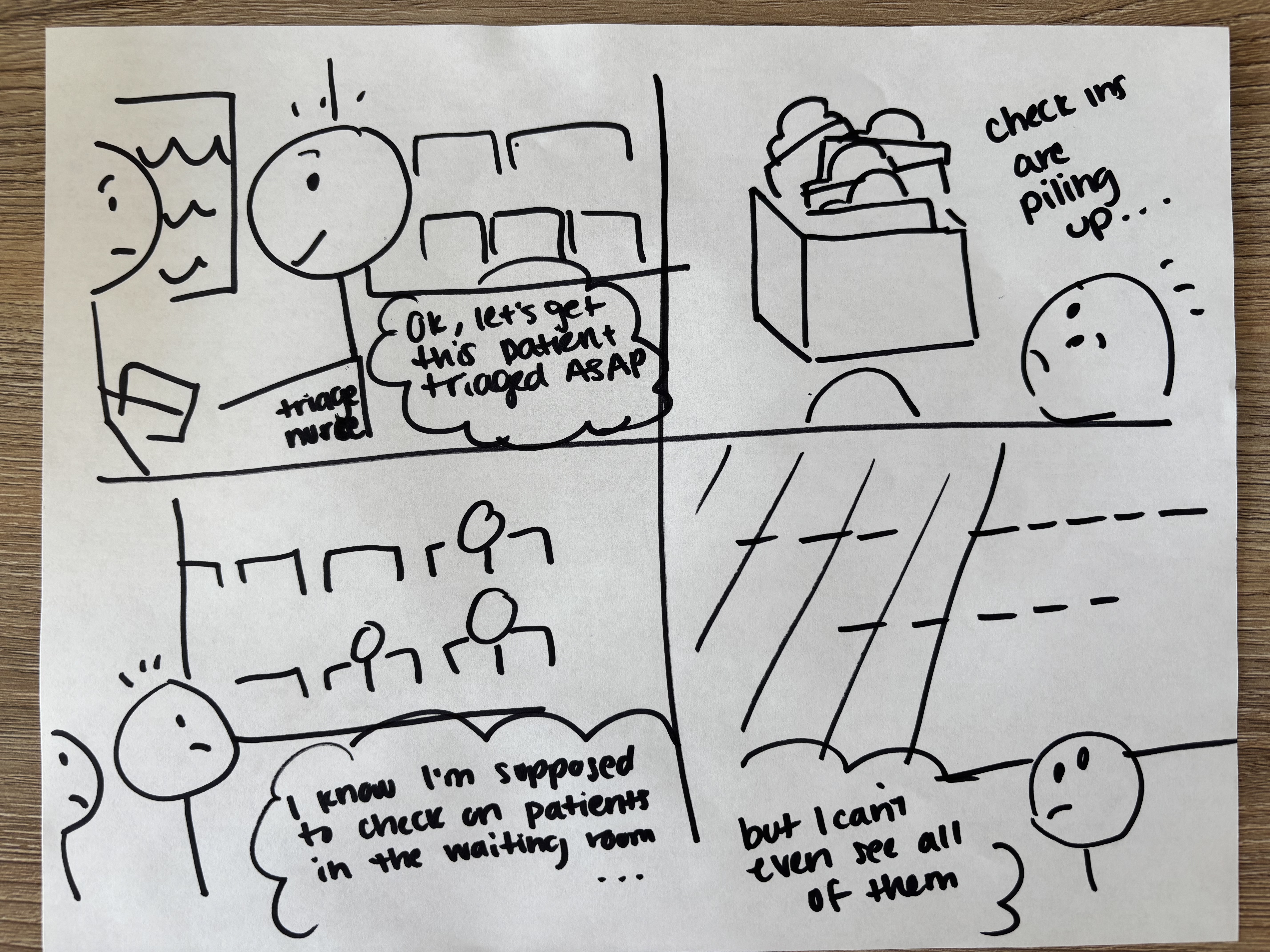
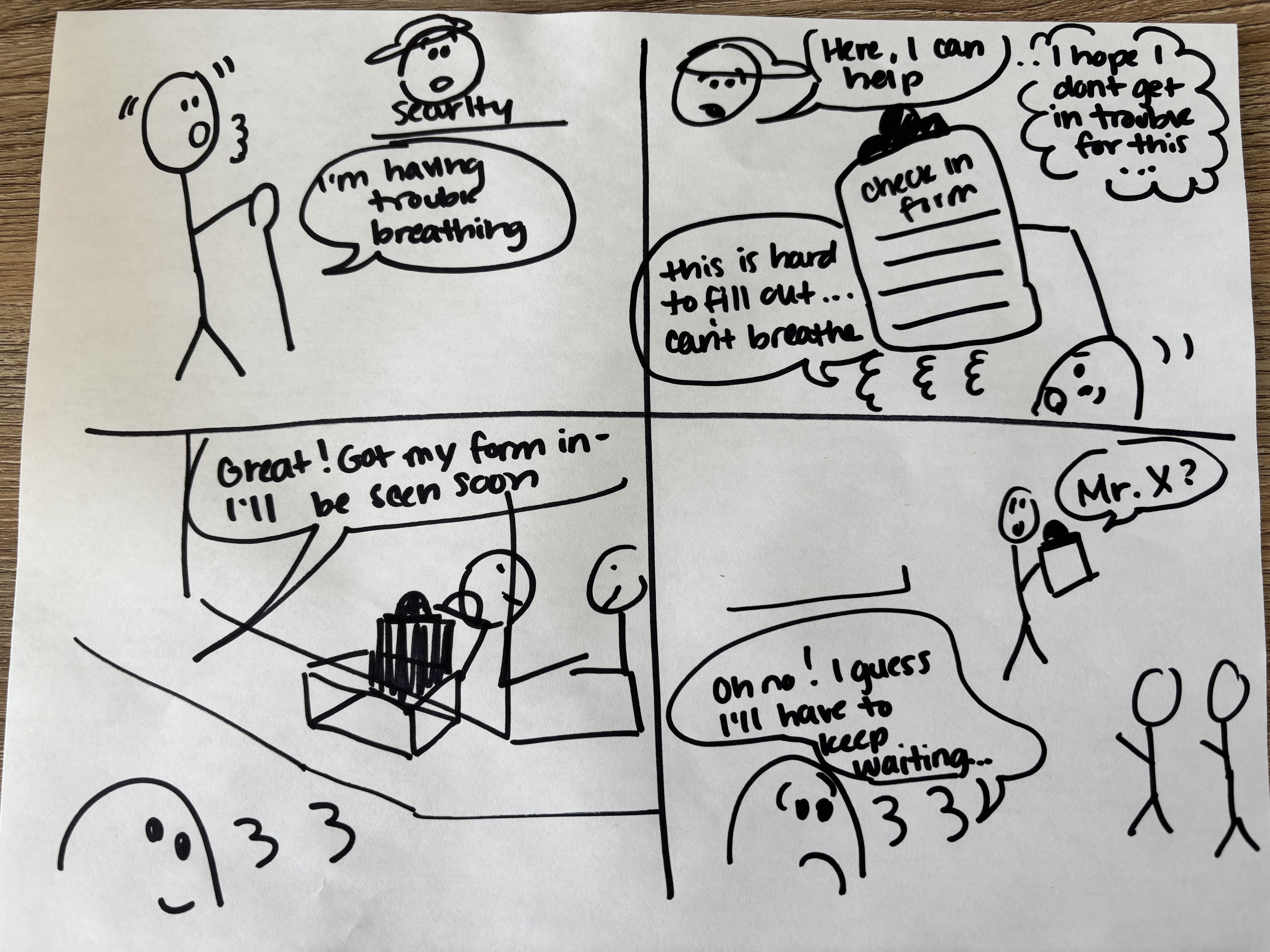
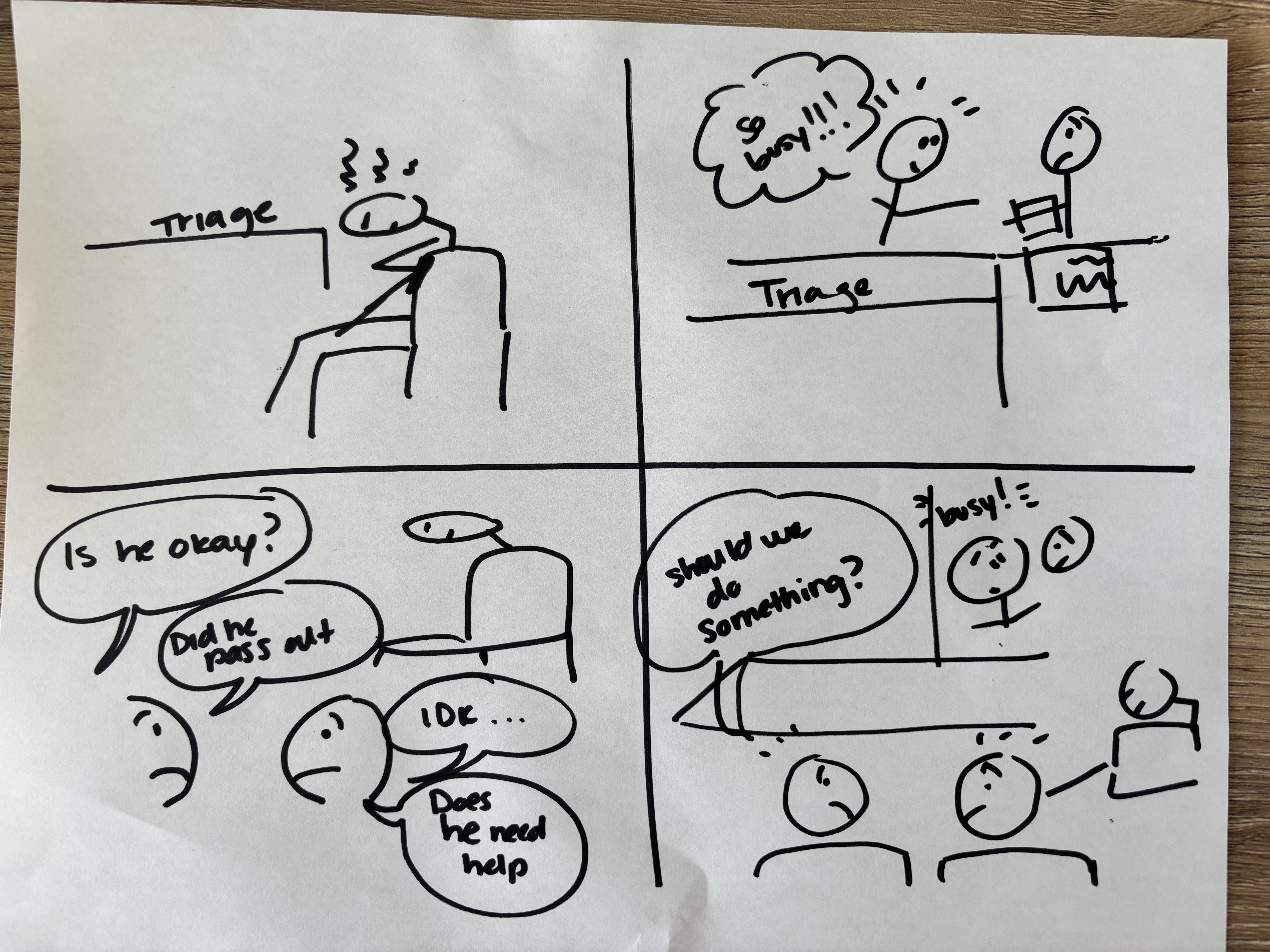
I deconstructed journey maps into key moments, then used storyboards to share key moments from the field study with our team. We used these storyboards to identify key opportunities that fueled our ideation kickoff.
We can't be too busy to protect patient dignity.
Our current privacy measures in the ED have created an unexpected challenge. The curtains and dividers that protect patient privacy also create this bubble where sound travels but sight doesn't. Staff and patients end up in this strange space where they can hear enough to be concerned but not enough to understand, leading to heightened anxiety on both sides and missed opportunities for early intervention.
Give providers permission and incentives to care.
Our ED staff consistently show they want to help - from security officers to techs - but they hit these invisible barriers of "scope" and "role." When a security officer sees someone struggling with paperwork, their instinct is to help, but our systems and culture often prevent this natural human response. We're seeing how these boundaries, created for operational clarity, end up fragmenting the care experience in ways that impact both staff fulfillment and patient care.
Help patients feel seen as soon as they walk in the front door.
Our triage nurses are caught in a complex dynamic - their efficiency in initial assessments directly increases the number of patients they need to monitor. Each successful triage adds another patient requiring observation, creating an escalating challenge that our current staffing model doesn't fully address. This isn't just about speed - it's about finding a sustainable way to maintain both rapid assessment and ongoing monitoring.
Let the patients be patients - not providers.
Patients and security staff are stepping into informal caregiver roles, watching out for each other when they sense staff are stretched thin. While this shows the incredible human capacity for care, it also signals a gap in our monitoring system that needs attention. The fact that patients feel this responsibility suggests our current staffing model isn't aligned with patient needs.
Ideation Kickoff
Using these insights, I helped facilitate a design thinking workshop with VCU Health leadership, providers, staff, VCU students, and community members to brainstorm ideas aimed at addressing communication gaps, helping patients feeling more cared for, reducing staff burn out, and making the wait more comfortable. Solutions were then prototyped through mockups and concept testing and refined with feedback from providers and staff.
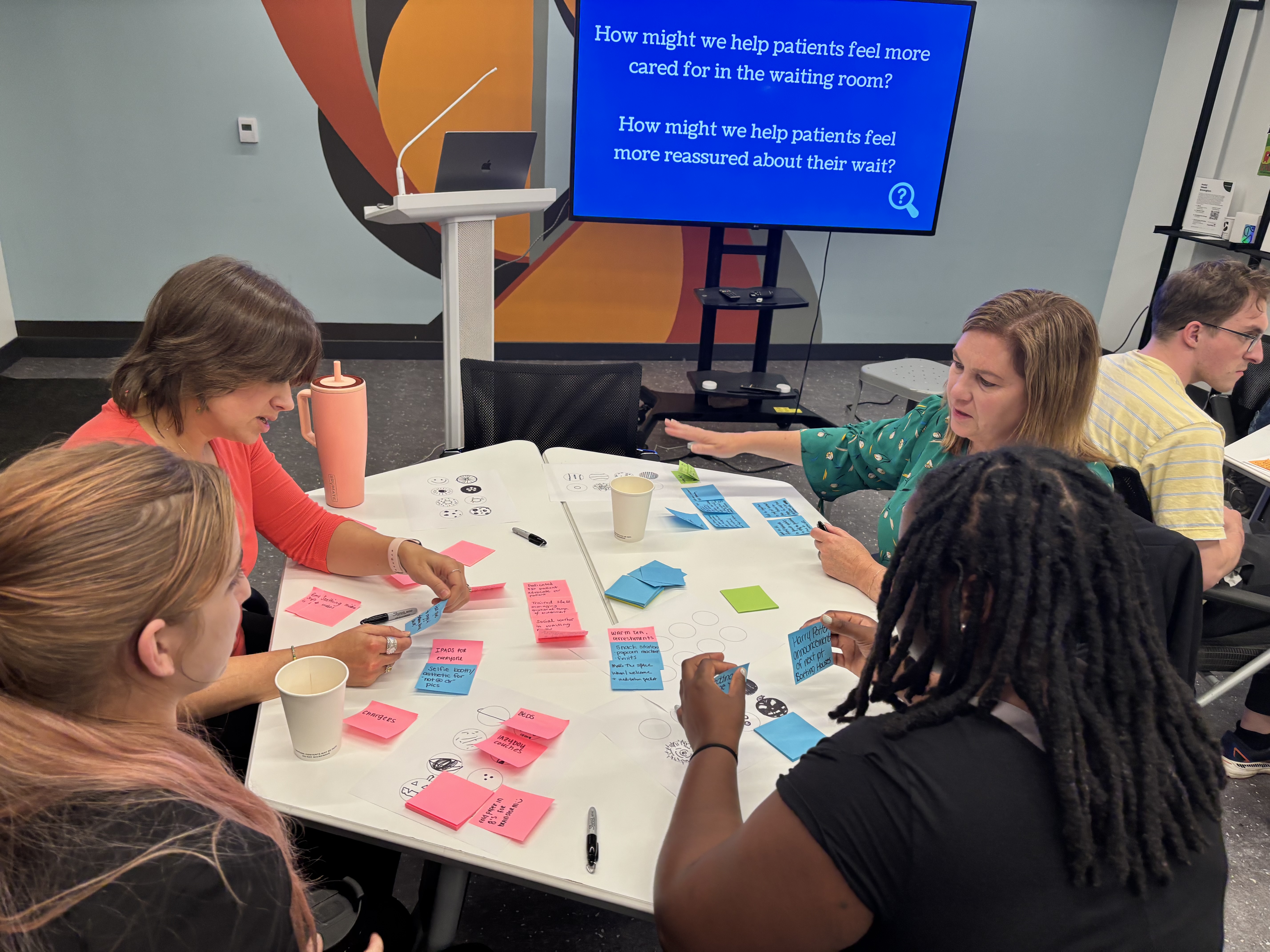
Students brainstormed alongside healthcare providers, staff, leadership, and community members to ensure many perspectives were included.
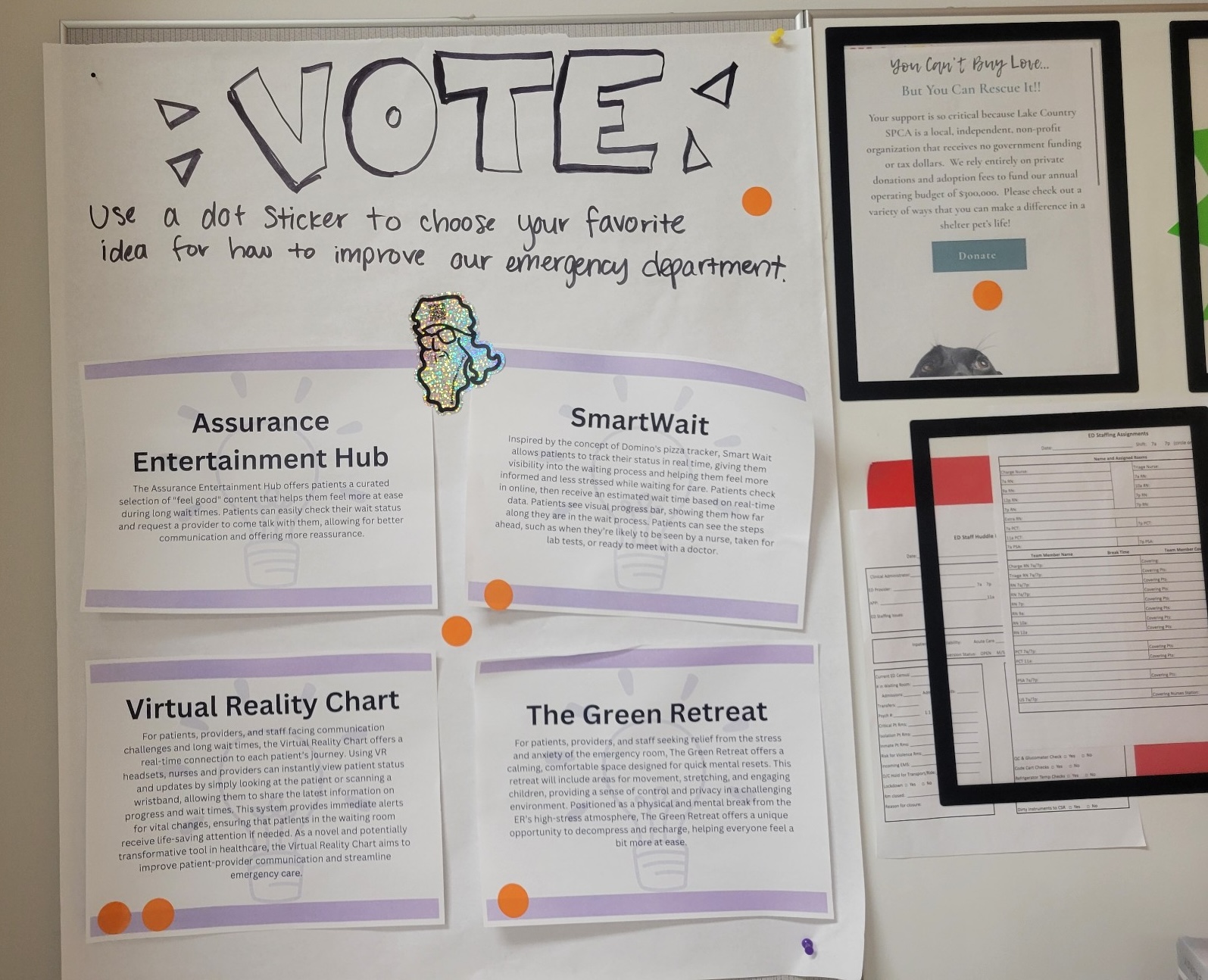
Dot Voting displays were used to collect directional feedback from patients, staff, and providers, while surveys were used for more detailed feedback.
The Results
While full implementation was not completed within the project timeline, our research and intervention testing led to tangible outcomes:
- 50% reduction in LWBS rates. Early metrics suggested a noticeable decline in patients leaving without being seen due to increased communication efforts.
- Enhanced staff awareness. Providers and leadership adopted a human-centered mindset, integrating patient communication strategies into their daily workflow.
- Cross-hospital knowledge sharing. I supported newsletter communications to share research findings and insights across both hospital sites, helping establish an ongoing dialogue on patient experience improvements.
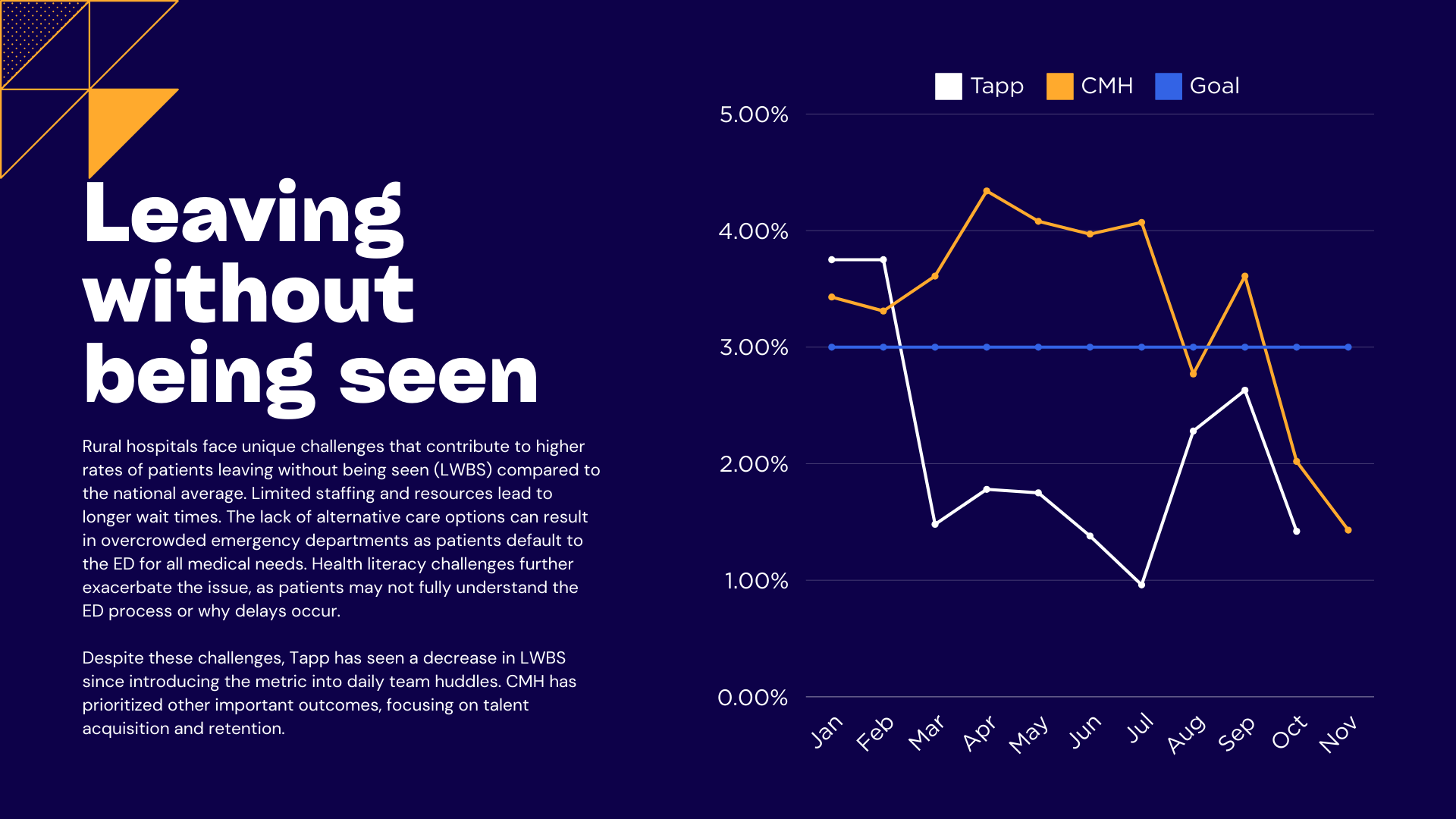
The number of patients leaving without being seen fell below the goal of 3% at both hospitals after we started working with the teams in September.
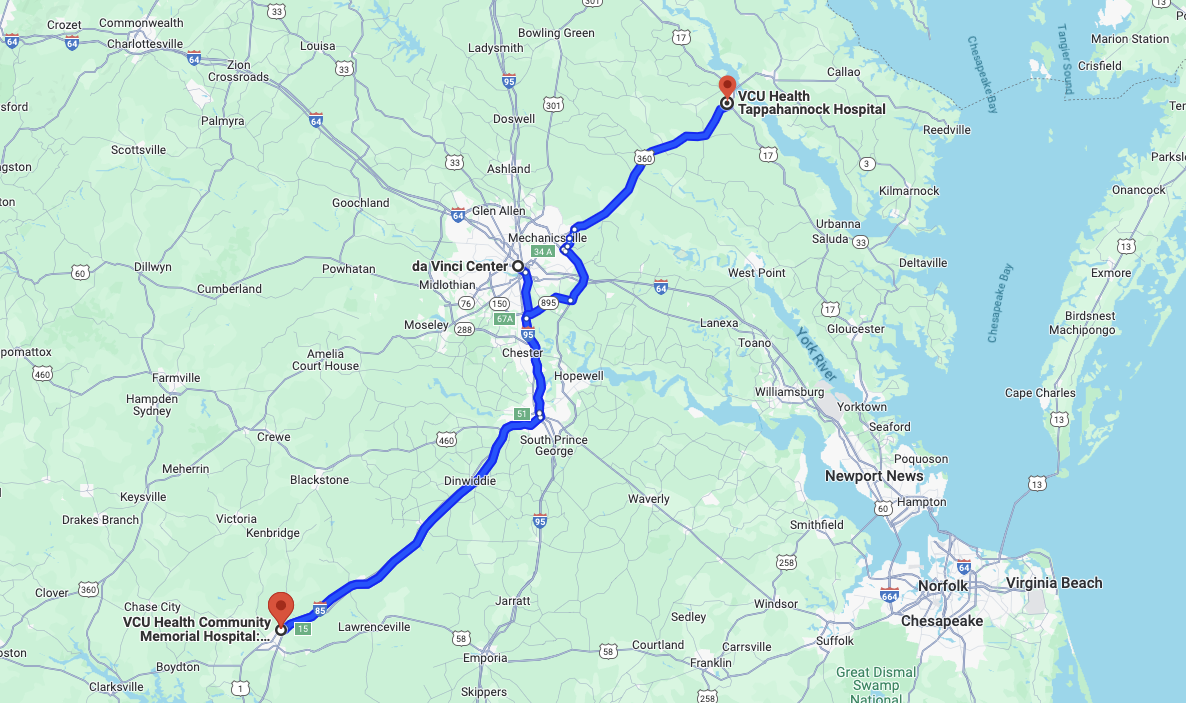
Insights are shared across both hospital sites, each of which has unique needs.
The VCU Student Experience
As part of this project, I co-taught the course “Designing the Future of Health” at VCU, which empowered students to tackle real-world challenges in rural health systems using design thinking. The course gave students hands-on experience in conducting field research, empathy interviews, and journey mapping, all while working alongside healthcare providers and hospital staff.
For their midterm presentations, students were understandably anxious about presenting to senior hospital leadership. This was their first time engaging with such a formal process, and most had little prior experience in healthcare or with the VCU Health System. However, these presentations turned into an incredible networking opportunity for the students, as they had the chance to share their research findings and opportunity statements directly with hospital administrators and senior leaders. The feedback they received not only validated their work but also opened doors for future collaboration.
At the end of the semester, we hosted a virtual demo day where students showcased their top ideas through engaging pitches. These presentations allowed students to demonstrate their creative thinking and problem-solving skills, leading to excitement from hospital staff about potential solutions moving forward.
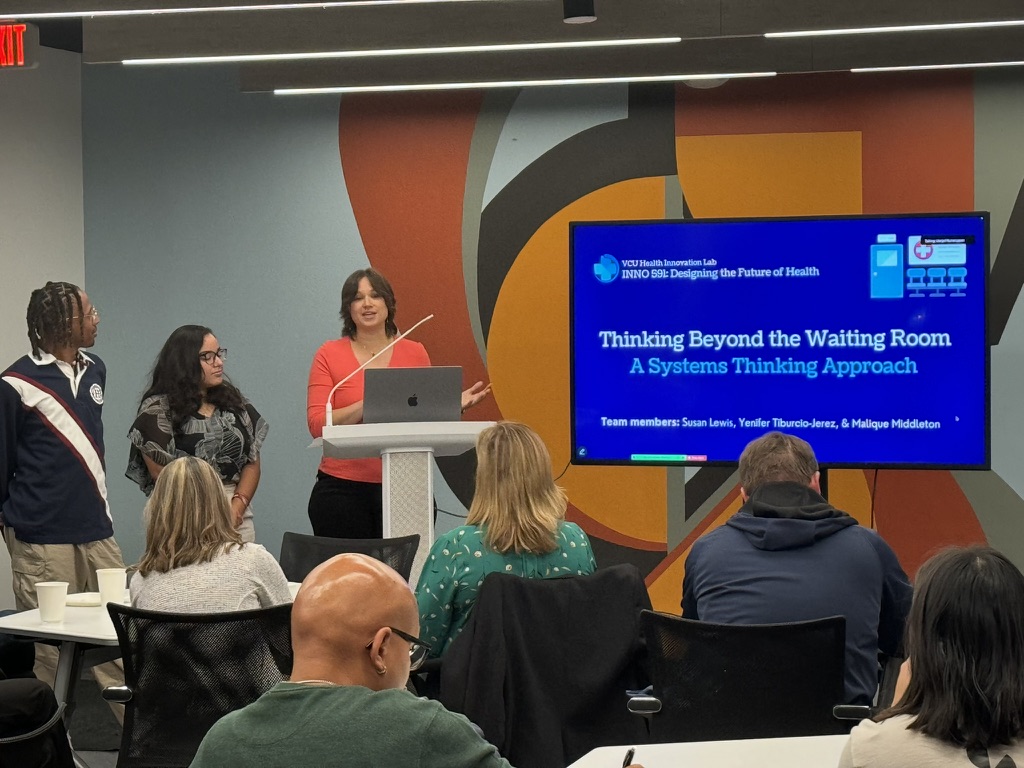
Students' midterm presentations to hospital leadership, providers, staff, and the Richmond community, allowed them to start a valuable dialogue and refine their understanding of the problem space before jumping into ideation.
Challenges Along the Way
- Teaching while being accountable for deliverables. It was difficult relying on students for consistent and timely deliverables, especially since it was their first time engaging with this process, and many had no prior experience in healthcare or with the VCU Health System.
- Limited patient representation. We were dependent on staff and provider engagement for collecting patient feedback, and despite our best efforts, we struggled to gain sufficient patient input to fully represent their experiences.
- Implementation schedule changes. While implementation was descoped from this semester, we did see considerable reductions in patients leaving without being seen. The feedback from providers, staff, and leadership about improved team morale was highly positive.
Looking Back
This project highlighted the power of empathy-driven, design thinking approaches to solving real-world healthcare challenges. It taught me valuable lessons in navigating resource constraints, fostering collaboration across teams, and using insights to advocate for meaningful change in healthcare. Even though we didn’t fully implement our solutions, the process brought fresh ideas, promoted communication, raised important issues for discussion, and improved morale among staff. By simply drawing more attention to the problem, we achieved real, measurable improvements in the number of patients leaving without being seen - an outcome that made this project a success in its own right.
On a personal level, this project reinforced the power of design thinking to bring diverse perspectives together to solve complex problems. Working alongside students who had no prior experience in healthcare allowed me to refine my facilitation skills and think creatively about how to bridge gaps between research, real-world application, and systemic change.